Uterine polyps are quite common. Almost 3 in 10 women may get them sometime in life, but not before turning 30. They often happen more around menopause. Uterine polyps are growths that stick out from the inner wall of the uterus. It happens when the lining of the uterus grows too much. Most of the time, these growths are not cancerous. But, sometimes, they can turn into cancer at later stages. Small polyps might not show any signs and can even disappear on their own.
Curious about the possibility of uterine polyps post-menopause? Let's unravel the answers together.
Can You Develop Uterine Polyps After Menopause?
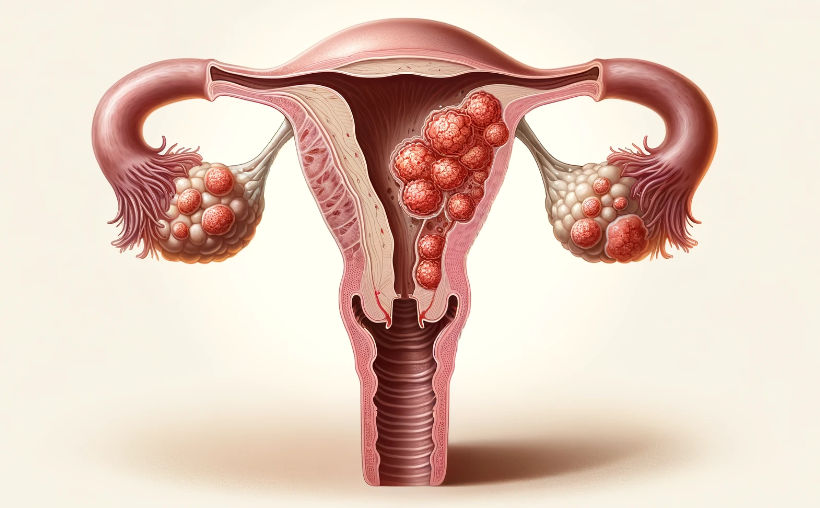
Yes, uterine polyps can develop after menopause. They are more commonly associated with women who are going through or have completed menopause. The risk of uterine polyps tends to increase with age. At the same time, they are less common in younger women. It is still possible for them to develop uterine polyps.
Can uterine polyps make an appearance after menopause? Prioritize your health—schedule your appointment now and stay ahead in understanding post-menopausal well-being.
Who is more likely to get affected by uterine polyps?
- Age as a Significant Factor: Uterine polyps are more likely to develop in individuals in their 40s and 50s, especially during the perimenopausal period.
- History of Hormonal Imbalances: Women who have a history of hormonal imbalances, such as excess estrogen, are more likely to have uterine polyps.
- Obesity: Being overweight (BMI 25 < 30) or obese (BMI > 30) increases the possibility of developing uterine polyps. Excess body fat can lead to hormonal imbalances, contributing to polyp formation.
- Connection to High Blood Pressure: Individuals with high blood pressure (hypertension) are at an elevated risk of uterine polyps.
- Tamoxifen Usage: Taking tamoxifen, a medication commonly used in breast cancer treatment, is associated with an increased risk of uterine polyps.
- Hormone Replacement Therapy: Women undergoing hormone replacement therapy with high doses of estrogen face a higher chance of developing uterine polyps.
- Inflammatory Conditions: Chronic inflammatory conditions of the uterus or cervix could increase the possibility of uterine polyps.
Let's navigate through the factors that could heighten the risk of uterine polyps after menopause!
What are the symptoms of uterine polyps after menopause?

- Unexpected Bleeding: If you notice any unexpected bleeding or spotting after menopause, it could be a sign of uterine polyps.
- Pelvic Discomfort: Some women may feel discomfort or pain in the pelvic area.
- Changes in Discharge: Pay attention to any changes in the color, consistency, or smell of the vaginal discharge.
- Feeling Full in the Pelvic Area: You might experience a sense of fullness or bloating in your pelvic region.
- Irregular Bleeding: Even if you've gone through menopause, experiencing irregular menstrual-like bleeding is a reason to see a doctor.
- Bigger Uterus: Uterine polyps sometimes make your uterus feel larger than usual. Your doctor can detect this during an exam.
Explore symptoms of uterine polyps post-menopause. Take charge of your health—contact us today and initiate a proactive approach to well-being.
Please remember, even if you're not sure, it's essential to talk to a doctor if you notice any unusual changes or symptoms. Regular check-ups with your gynecologist are a good way to stay on top of your health, especially after menopause.
Delve into the science behind uterine polyps after menopause!
Why Do Uterine Polyps Occur After Menopause?

Uterine polyps can occur after menopause due to hormonal changes. Low levels of estrogen and progesterone are found in the body after menopause. There is a decline in hormone levels. However, some women may still have small amounts of estrogen. This residual estrogen can stimulate the lining of the uterus (endometrium) to grow. It leads to the development of uterine polyps after menopause.
What Are the Risk Factors for Uterine Polyps After Menopause?
Certain factors increase the risk of uterine polyps after menopause. They include:
- Going through perimenopause or postmenopause.
- Being overweight.
- Using tamoxifen. It is a medication taken for breast cancer.
Curious about the diagnostic journey? Join us as we explore the various methods and procedures used to unveil the presence of uterine polyps after menopause!
How Are Uterine Polyps Diagnosed After Menopause?

Your doctor will examine your health history, symptoms, and medications during your appointment. If you are already at the menopause stage, the doctor may discuss about unusual bleeding etc. To gain insights, pelvic function and a pap smear will be conducted. Additional diagnostic methods may include:
- Transvaginal Ultrasound: A healthcare professional will place a small device in your vagina, emitting sound waves to create an image of your uterus.
- Sonohysterography: A procedure that introduces fluid into the uterus to enhance the ultrasound image.
- Hysteroscopy: Your doctor inserts a thin tube with a lighted telescope through your vagina to examine the uterus.
- Endometrial Biopsy: During this process, your doctor collects tissue for laboratory testing.
- Curettage: A metal instrument is used to gather tissue, which is then sent to the lab for examination.
Discover how uterine polyps are diagnosed post-menopause. Take the first step to recovery—get in touch with us for your treatment and embark on a journey to well-being.
Understanding these procedures helps your doctor make informed decisions about your health.
Get ready to discover the array of options available for managing uterine polyps after menopause!
What Are the Treatment Options for Uterine Polyps After Menopause?

The treatment of uterine polyps after menopause depends on your symptoms. If you are having menopause and uterine polyps are causing problems, you might need treatment. The treatment options include:
- Medications: Drugs to balance hormones can be used to relieve symptoms. But once you stop the medicine, they may return.
- Uterine polypectomy: The doctor can remove the polyp during a hysteroscopy. A tool is used to cut and remove it precisely. Then, the tissue will be sent to a lab for testing. If the polyp is cancerous, the doctor may recommend a hysterectomy.
Empower yourself with insights into the manageability of uterine polyps after menopause!
Are Uterine Polyps After Menopause Manageable?
Yes, uterine polyps after menopause are manageable. Most of the time, uterine polyps go away by themselves. Regular monitoring without intervention is enough if the polyps are not causing problems. If symptoms arise, then medications are needed. Sometimes, uterine polypectomy is also considered. The approach to treatment depends on the individual and the risk factors. Regular checkups and open communication with your doctor are required for the same.
Explore the manageability of uterine polyps after menopause. Your well-being is our priority—call us to book your appointment today and secure a path to proactive health management.
Join us in unravelling lifestyle changes and proactive steps to potentially reduce the risk of uterine polyps after menopause. Let's explore the strategies for a healthier tomorrow.
Can Uterine Polyps After Menopause Be Prevented?
Prevention of uterine polyps after menopause is not guaranteed. Having regular checkups with your gynaecologist helps to detect them early. This may prevent some severe complications that can arise due to uterine polyps.
Specific lifestyle changes help to reduce the risk. Maintain a healthy weight and stay physically active. You can avoid prolonged use of hormone therapy for menopause symptoms. It is also a reason for developing uterine polyps after menopause.
References: