Overview
Seizures can occur as a complication following brain surgery, affecting a significant number of patients. These postoperative seizures are often a result of the brain's response to surgical trauma, changes in brain tissue, or irritation at the surgical site. Seizures are more likely to occur in the immediate postoperative period (within 2 weeks of surgery) Managing seizures post-surgery is crucial for recovery, requiring close monitoring and tailored treatment plans.
Seizures can impact a patient's recovery and quality of life, making early detection and effective management essential.
Are you or a loved one struggling with seizures after brain surgery? You're not alone. Book your appointment with the best neurosurgeons in India for expert tips and advice.
The risk of seizures after brain surgery is higher in patients with preexisting seizure disorders. Also, it is important to note that in those who have undergone many surgeries, other risk factors for postoperative seizures include age, the type of surgery, and the presence of residual tumors.
Did you know?
Is it common to have a seizure after brain surgery?
According to the National Center for Biotechnology Information (NCBI), seizures after brain surgery are not uncommon. However, the frequency of seizures varies depending on the type of surgery and the underlying condition.
- Seizures after meningioma removal or brain tumor removal may be more common than seizures after other types of brain surgery.
- The likelihood of seizures after craniotomy also varies depending on the location of the tumor and the extent of the surgery.
- Other studies have shown the incidence of seizures is higher in patients who underwent open surgery compared to those who underwent minimally invasive or endoscopic surgery.
In some cases, seizures may resolve on their own after brain surgery. In other cases, seizures may persist or get even worse. However, seizures can occur as a side effect of brain surgery, but it is not common.
An experienced Dr. James Walker a clinical doctor with over many years of experience, has quoted that -
“The most common type of seizure seen after brain surgery is a partial seizure, which originates from a specific part of the brain. These seizures cause various symptoms, like muscle twitching, numbness, or changes in sensation. Generalized seizures that involve the entire brain can also occur after brain surgery. Anti-seizure medications are used as a treatment for seizures after brain surgery, like phenytoin, carbamazepine, or levetiracetam.”
Do seizures go away on their own after brain surgery?
Seizures following brain surgery that isn't specifically aimed at treating epilepsy may or may not disappear on their own. The outcome depends on various factors, such as
- Type of Surgery: The specific surgical procedure performed on the brain can influence whether seizures go away on their own.
- Underlying Condition: The brain condition that led to surgery can also influence if seizures resolve.
- Individual Response to Treatment: Each person's response to treatment, including medication and rehabilitation, plays a crucial role in determining whether seizures persist or resolve after brain surgery.
Causes of a seizure after brain surgery
- Damage during surgery: Brain tissue may get damaged or disturbed, leading to seizures.
- Inflammation or infection in the brain can lead to seizures, as the brain's electrical activity is affected.
- Post-operative bleeding or hematoma: Bleeding or hematoma can cause pressure on the brain and lead to seizures.
- Changes in the brain's electrical activity: The brain's electrical activity can be changed after surgery, leading to seizures.
- The underlying condition that prompted the surgery: The brain tumor treatment that prompted the surgery may cause seizures even after the surgery.
How does the location of brain surgery affect post-surgical seizures?
Dr James Walker, says that -
"The location of the surgery within the brain can affect the likelihood of post-surgical seizures. Surgeries that involve the temporal lobe or the frontal lobe of the brain are associated with a higher risk of seizures. In contrast, surgeries that involve the occipital lobe or the cerebellum are associated with a lower risk of seizures."
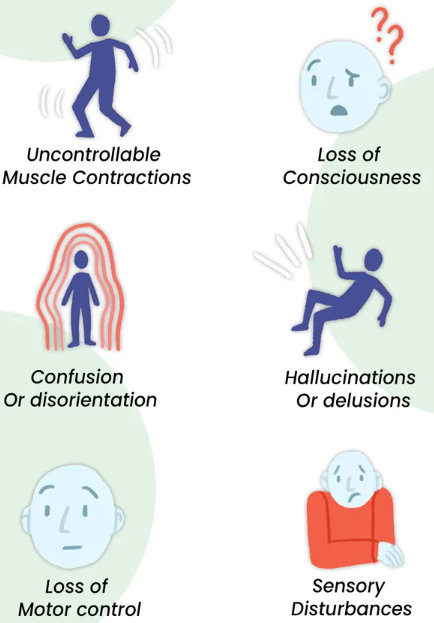
Symptoms of seizures after Brain Surgery
Symptoms of seizures after brain surgery vary depending on the individual and the underlying cause of the seizures.
Seizures have different symptoms depending on the type of seizure and the area of the brain affected. Not all people will have the same symptoms.
Can you relate to any of the above symptoms? Get in touch with the specialist for a free consultation at the earliest for proper diagnosis and treatment!
Brain surgery is a big step - but what happens when seizures become a hurdle?
Diagnosis of seizures after Brain Surgery
The first step in diagnosing seizures is to obtain information about the brain surgery, symptoms the patient has experienced, and other relevant medical conditions. The doctor will also perform a physical examination to check for signs of seizures, such as muscle contractions or changes in consciousness.
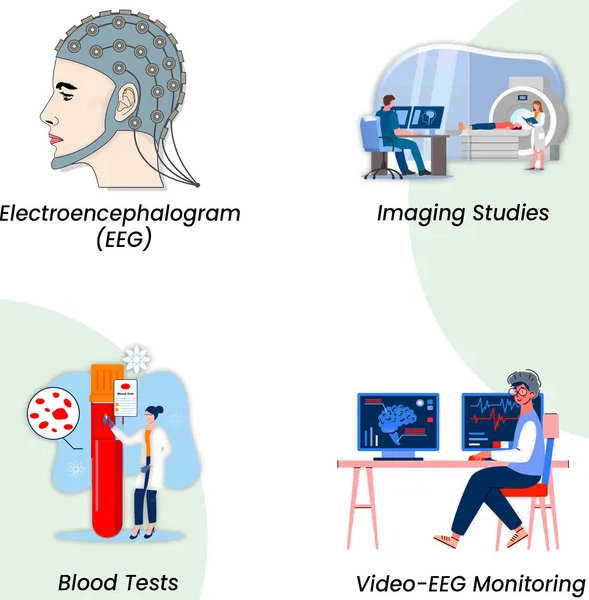
| This test records the electrical activity of the brain. It can help identify abnormal patterns associated with seizures. |
| CT or MRI scans can be used to look for any abnormalities in the brain that may be causing seizures. |
| These can be used to check for any underlying medical conditions that may be contributing to seizures. |
| This test records the person's seizures and the accompanying brain activity, allowing for more accurate diagnosis and treatment. |
"Seizures after brain surgery can be a challenging but manageable complication. They often result from the brain's response to surgical trauma or irritation at the surgical site. Effective management through medication and regular monitoring is crucial to ensure a smooth recovery and minimize the impact on the patient's quality of life." says Dr. Gurneet Sawhney, a renowned Neurosurgeon.
Treatment of seizures after Brain Surgery
Treatment for seizures after brain surgery involves
Anti-Seizure Medication:
Anti-seizure medication is the most common treatment for seizures after brain surgery. The type of medication prescribed will depend on the type of seizure and the underlying condition that prompted the brain surgery. The goal of anti-seizure medication is to reduce the frequency and severity of seizures and improve the person's quality of life.
Surgical Options:
- In some cases, surgery may be required to remove any abnormal brain tissue that is causing the seizures. The treatment of seizures after brain surgery depends on the underlying cause of the seizures and the person's case.
- Implantable Devices: Sometimes, devices like a vagus nerve stimulator are implanted to help control seizures. These devices send regular, mild pulses of electrical energy to the brain via the vagus nerve.
Deep Brain Stimulation (DBS):
- DBS is a treatment option for some patients with hard-to-control seizures. It involves implanting electrodes in specific parts of the brain.
- These electrodes send electrical impulses to regulate abnormal brain activity, which can help reduce the frequency and severity of seizures.
Lifestyle Changes:
- In some cases, lifestyle changes may also be recommended to help reduce the risk of seizures. For example, if a person has a history of seizures triggered by sleep deprivation or alcohol consumption, they are advised to get enough sleep and avoid alcohol.
Risks or complications of seizures after brain surgery
Injury: Seizures can cause injury to the brain or other parts of the body, such as broken bones, bruises, or cuts.
Prolonged recovery: Seizures can prolong recovery time and impede the healing process.
Development of chronic seizures: Recurrent seizures lead to the development of chronic seizures and an increased risk of seizures in the future.
Cognitive and emotional difficulties: Seizures can also lead to cognitive and emotional difficulties such as memory loss, confusion, depression, and anxiety.
Medication side effects: Anti-seizure medications can have side effects such as drowsiness, confusion, dizziness, and nausea.
Loss of Independence: Seizures can lead to loss of independence and a change in the quality of life for patients and their families.
Increased mortality risk: Seizures can increase risk due to injury or other complications.
Can seizures after brain surgery become chronic?
Yes, seizures following brain surgery can indeed become chronic, depending on several factors:
- Surgery Scars: Scar tissue in the brain from surgery can become a spot where seizures start, possibly causing ongoing seizures.
- Initial Issue: If the reason for the surgery (like a tumor or abnormal blood vessels) is linked to epilepsy, seizures might keep happening even after surgery.
- Incomplete Removal: If not all the epilepsy-related tissue is taken out during surgery, seizures could still occur.
Don't let seizures and their risks hold you back from undergoing brain surgery - learn how to take control of seizures with preventive measures.
Preventing post-brain surgery seizures
- Medication: Take prescribed antiepileptic drugs as directed to prevent seizures.
- Regular Monitoring: Attend follow-up appointments for regular check-ups and monitoring.
- Healthy Lifestyle: Maintain a balanced diet, sleep well, and manage stress.
- Avoid Triggers: Identify and avoid potential seizure triggers such as flashing lights, lack of sleep, and excessive alcohol.
- Hydration: Stay well-hydrated to support overall brain health.
- Adhere to Care Plan: Follow your healthcare provider’s post-surgery care plan closely.
- Support System: Engage with a support system for emotional and practical support.
Learn how to manage seizures after brain surgery with our comprehensive guide. Schedule your Consultation with the top neurosurgeon for guidance and effective treatment options.
Prognosis of Brain Seizures After Surgery
The prognosis for seizures after brain surgery can vary depending on the underlying cause and the severity of the seizures. In some cases, seizures may resolve on their own or with treatment. Yet, in other cases, seizures may persist or even worsen. Close monitoring and follow-up with a skilled surgeon are required.
References: