Let’s take a look at the incidence of people having a stroke and seizure at the same time.
Various studies have reported higher rates of seizures in certain subgroups of stroke patients. The subgroup includes those with a stroke in the temporal lobe of the brain or those with a history of seizures before the stroke.
- According to 2018 research, seizures occurred in 9.3% of stroke patients overall.
- Some studies have reported a higher incidence of seizure after stroke in patients with hypertension, diabetes, and other risk factors.
- The incidence of seizures in temporal lobe stroke patients can range from 10-20%. In some studies, it has been reported that up to 30% of patients with temporal lobe stroke experience seizures. A temporal lobe stroke occurs on the sides of the brain, just above the ears.
- According to studies, about 5-10% of patients who have had an ischemic stroke will experience post stroke seizure within the first 7 days after the stroke. This rate increases to about 20-30% within the first 2 weeks after the stroke. An ischemic stroke occurs due to a blockage in a blood vessel.
- In Hemorrhagic stroke, a stroke due to a bleed in the brain, the incidence of seizures is lower, around 1-2%.
It is worth noting that these numbers can vary depending on:
- the population studied
- the inclusion criteria of the study, and
- the definition of seizures used in the study
Overall, please remember that the incidence of seizures after a stroke is not insignificant. Patients with a recent stroke should be evaluated for seizures and monitored for the development of post stroke seizure.
To get the best treatment you need to get help from the top hospitals in India.
Do stroke cause seizures?
A stroke and a seizure can be related in certain circumstances. A stroke can cause seizures if it affects the part of the brain that controls seizures. This is known as post stroke seizure or acute symptomatic seizures.
These seizures usually:
- occurs within the first 7 days after a stroke.
- occurs in about 5-10% of patients who have had a stroke.
Additionally, a stroke can increase the risk of developing seizures in the future.
Studies have shown that people who have had a stroke are more likely to develop epilepsy. Post stroke epilepsy is a condition characterized by recurrent seizures. Although epilepsy and stroke are two distinct medical conditions, but they can be related in some cases. This is especially true if the stroke occurs in the temporal lobe of the brain. The temporal lobe is the area of the brain that is most commonly associated with seizures.
Note: Stroke and seizures can also occur independently and are not related to each other. Therefore, it is important to seek medical attention immediately if you suspect that you or someone else is experiencing either of these conditions.
There are various types of seizures that you may be unaware of. Here we have it for you.
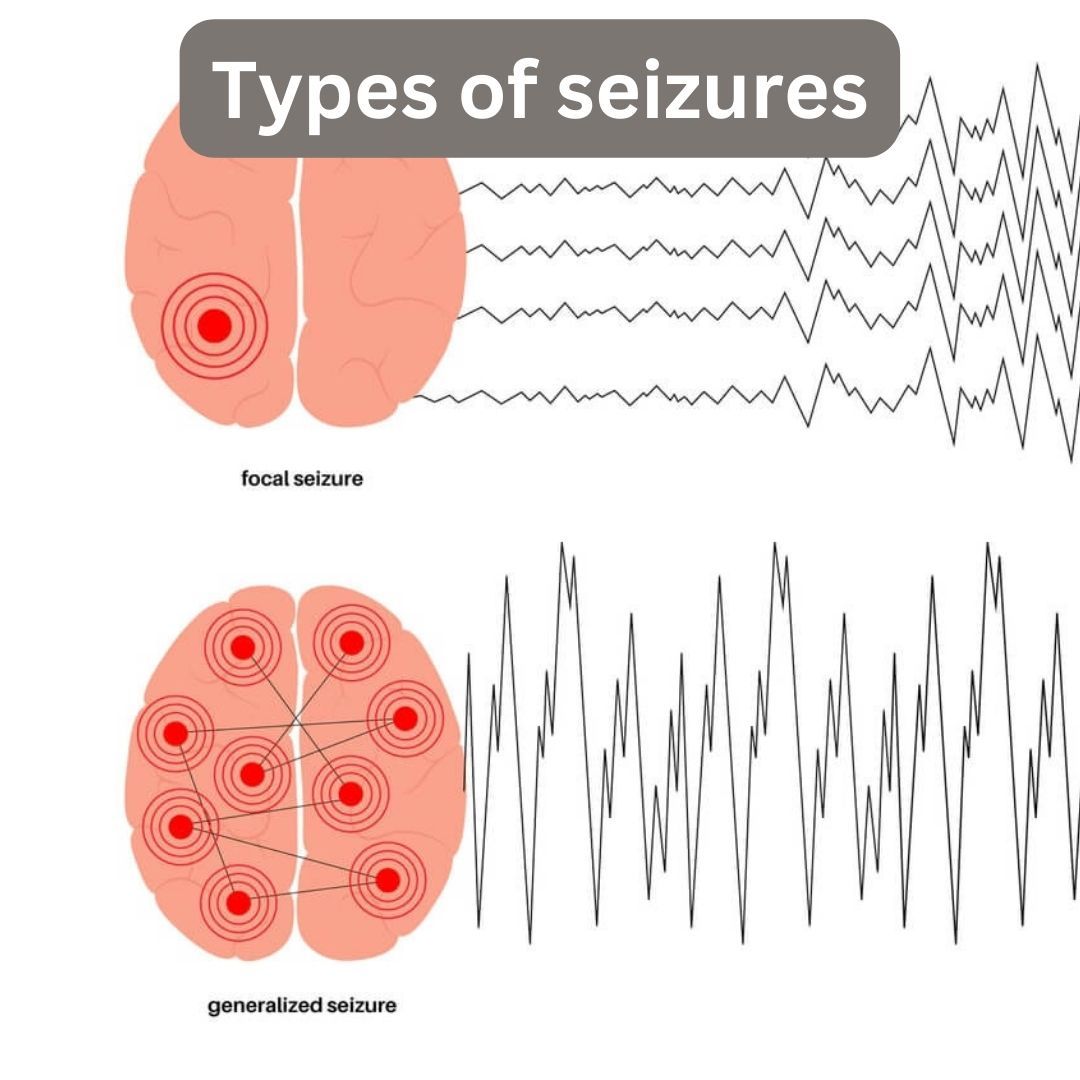
What are the types of seizures:
There are several different types of seizures, which can be classified based on their characteristics and the part of the brain they affect. These symptoms are based on the type of seizure you have. Some of the most common types of seizures include:
- Focal seizures: Also known as partial seizures, these seizures affect a specific part of the brain and can cause changes in sensation, movement, or emotions. Focal seizures can be further classified as simple or complex, depending on whether consciousness is affected.
- Generalized seizures: These seizures affect both sides of the brain and typically involve loss of consciousness. There are several different types of generalized seizures, including:
- Absence seizures: Brief episodes of staring or absence of awareness that may be mistaken for daydreaming.
- Tonic-clonic seizures: Also known as grand mal seizures, these seizures involve a loss of consciousness, stiffening of the body, and convulsions.
- Atonic seizures: These seizures involve sudden loss of muscle tone, causing the individual to fall to the ground.
- Unknown onset seizures: Some seizures may be classified as unknown onset if it is unclear where in the brain the seizure started, or if the individual was not aware of the seizure when it began.
- Reflex seizures: These seizures are triggered by specific stimuli, such as flashing lights or loud noises.
- Psychogenic non-epileptic seizures (PNES): These seizures resemble epileptic seizures but are not caused by abnormal electrical activity in the brain. PNES are thought to be related to psychological or emotional factors.
A stroke sounds concerning enough, but the thought of having a stroke and seizure at the same time sounds scary, doesn’t it? Let’s find out the consequences of having this dual occurrence.

Is it dangerous to have a co-occurring stroke and seizure?
Having a stroke and a seizure together can be dangerous, as both conditions can cause brain damage and loss of function.
| Stroke | Seizure | Dual occurrence |
A medical emergency where the blood supply to the brain is disrupted. It can cause:
| A sudden electrical disturbance in the brain can cause:
| The combined effects of the two conditions can be particularly severe.
|
Please remember early diagnosis and treatment can help to minimize the risk of complications and improve the chances of recovery.
What type of stroke causes seizures to occur at the same time?
A stroke that affects the brain's temporal lobes can cause seizures to occur at the same time. This type of stroke is known as a temporal lobe stroke. It can occur due to a disruption of blood flow to the temporal lobes. It can lead to damage or injury to this area of the brain.
The temporal lobes are responsible for crucial functions such as memory, language, and emotion. A stroke in this area can cause a wide range of neurological symptoms, including seizures.
Overall, having a stroke and a seizure together can be dangerous and require prompt medical attention.
So, how can you recognize if you are having a stroke and seizure at the same time? Let’s find out the symptoms of these conditions.
To find out the same you may also need to consult the best Neurology hospitals in India.
What are the various symptoms of stroke and seizure that occur simultaneously?
Symptoms of the occurrence of stroke and seizure at the same time can vary depending on the location and severity of the brain injury. However, some common symptoms that may be experienced include:
| Loss of consciousness | |
| Confusion | |
| Numbness or weakness on one side of the body | |
| Difficulty speaking or understanding speech | |
| Vision problems in one or both eyes | |
| Dizziness or loss of balance | |
| Headache or neck pain | |
| Seizures or convulsions | |
| Memory problems or difficulty with other cognitive functions | |
| Bladder and bowel issues |
Note: These symptoms can also occur individually and may not be related to a stroke or seizure. Regardless, if you or someone you know is experiencing any of these symptoms please do not delay seeking medical attention.
What can cause stroke and seizure to occur at the same time?
A stroke can cause a seizure if:
- it affects the brain in a way that disrupts normal electrical activity.
- it damages or destroys brain tissue.
- it causes a lack of oxygen or blood flow to the brain.
- it affects the part of the brain that controls seizures.
Also, a patient who has had a stroke may have an increased risk of developing seizures. In this case, a seizure can occur as a complication of stroke and may be referred to as a post stroke seizure. This type of seizure can occur within days, weeks, or months after a stroke.
Additionally, certain medical conditions, such as brain tumors or infections, can cause both stroke and seizures to occur at the same time.
If you are wondering how a stroke can increase your chances of having a seizure, please continue reading to find out.
How does a stroke increase the risk of seizures at the same time?
A stroke can increase the risk of seizures in several ways.
- A stroke can damage the brain, leading to seizures by altering the normal electrical activity in the brain.
- Strokes caused by bleeding in the brain (hemorrhagic stroke) can cause increased pressure within the skull, which can also lead to seizures.
- Certain medications used to treat stroke can also increase the risk of seizures.
A person who has had a stroke may be more susceptible to seizures due to other underlying health conditions or risk factors.
Yes, there are certain short term & long term effects that you need to understand, keep reading further.

Short term & long term effects of stroke and seizures
Multiple seizures and having epilepsy can have both immediate and long-term consequences. These can include everything from a decline in the quality of living to an increase in the risk of mental health issues.
| Short-term effects of stroke | Long-term effects of stroke |
|
|
| Short-term effects of seizures | Long-term effects of seizures |
|
|
Let’s understand how the occurrence of a stroke and seizure at the same time is diagnosed.
Diagnosing the co-occurrence of stroke and seizure
The diagnosis of a stroke and a seizure occurring simultaneously can be challenging, as the symptoms of these two conditions can overlap. However, there are some key differences in the symptoms that can help doctors make a diagnosis.
In the case of a stroke, symptoms may include:
- sudden weakness or numbness on one side of the body
- difficulty speaking or understanding speech
- vision problems
- severe headache
In the case of a seizure, symptoms may include:
- heat stroke convulsions
- loss of consciousness
- muscle contractions
- changes in behavior
Doctors may use a combination of the following tests to diagnose a stroke and seizure. Find the best neurologists and cardiologists in India here.
Physical examination | Physical examination includes assessing the patient's level of consciousness, speech, muscle strength, and coordination.
|
Neurological examination | A neurological examination involves assessing the patient's mental status, reflexes, sensations, movement, and coordination.
|
Imaging tests (CT or MRI scans) | Imaging tests can provide detailed images of the brain and reveal any structural abnormalities, bleeding, tissue death or damage. |
Electroencephalogram (EEG)
| EEG is a test to measure and record the electrical activity of your brain. |
Blood tests | Blood tests may also be done to check for any underlying medical conditions or infections that could be causing the symptoms. |
Note: In some cases, it can be difficult to distinguish between the symptoms of a stroke and those of a seizure. Prompt medical attention is important for proper diagnosis and treatment.
Are you wondering about the treatment and management of having a stroke and seizure at the same time? Let’s take a look.
Treatment of stroke and seizure occurring simultaneously
The treatment and management of a stroke and a seizure occurring simultaneously will depend on the specific type of stroke and seizure, as well as the underlying cause.
| Ischemic stroke | Ischemic stroke is caused by a blocked blood vessel. Treatment may include administering a clot-busting medication, such as a tissue plasminogen activator (PLAT or tPA), and medications to lower blood pressure and cholesterol to reduce the risk of further strokes. |
| Hemorrhagic stroke | Hemorrhagic stroke is caused by bleeding in the brain. Treatment may include medication to lower blood pressure and control the bleeding, as well as surgery to remove the blood clot or repair the damaged blood vessel. |
| Seizures | Seizures are caused by interruptions in the connection between the brain and nerve cells. Treatment may include medications such as anti-seizure drugs to control seizures, and surgery to remove any underlying brain lesion that may be causing seizures. |
Recovery after a post-stroke seizure
Rehabilitation is an important part of treatment and recovery after having a post-stroke seizure. This will include physical therapy, occupational therapy, and speech therapy to help the patient recover as much functionally as possible.
As mentioned earlier, stroke and seizure both are serious conditions and require prompt medical attention. Please ensure that treatment is started as soon as possible after diagnosis. The treatment plan will be tailored to the individual patient and may need to be adjusted as the patient's condition changes.
Let us understand how you can lower the risk of having a seizure after a stroke.

Tips to prevent a post-stroke seizure
Preventing a post-stroke seizure may involve addressing underlying medical conditions and risk factors that increase the likelihood of both conditions.
Control hypertension | High blood pressure is a major risk factor for stroke, so keeping blood pressure under control can help reduce the risk of stroke.
|
Manage diabetes | People with diabetes are at higher risk of stroke and seizures, so managing blood sugar levels can help reduce the risk of both conditions.
|
Treat and prevent atrial fibrillation | Atrial fibrillation is a type of heart rhythm disorder that can increase the risk of stroke and seizures.
|
Control cholesterol levels | High cholesterol levels can increase the risk of stroke and seizures. Controlling cholesterol levels through diet, exercise, and medication can help reduce the risk of both conditions.
|
Avoid smoking and excessive alcohol consumption | Smoking and excessive alcohol consumption can increase the risk of stroke and seizures. So try and quit smoking and if you have to drink, drink moderately.
|
Maintain a healthy diet | Eating a diet that is high in fruits, vegetables, and whole grains, and low in saturated fat and cholesterol can help reduce the risk of stroke and seizures.
|
Regular exercise | Regular exercise can help reduce the risk of stroke and seizures by improving cardiovascular health and controlling blood sugar levels. |
Take medication as prescribed | If you have been prescribed medication to prevent or treat seizures or stroke, it is important to take it as directed. |
But what can you do to help someone who is having a post-stroke seizure before the arrival of a health professional? Don’t worry, read on to understand how you can help.
Here’s what you can do to help someone through their seizure:
Here are some first aid steps that you can take to help someone who is having a seizure:
- Clear the area around the person of any sharp or hard objects that could cause injury.
- Place something soft, such as a jacket or blanket, under the person's head to protect their brain from further injury.
- Loosen or adjust any clothes that seem to be too constricting around their neck.
- Do not try to restrain the person unless they run the risk of injuring themselves.
- Don't put anything in their mouth.
- Turn or position the seizure patient on their side to help prevent gagging and vomiting.
- Stay with the person until the seizure has ended and they are fully awake.
- Don't offer food or drink until the person is fully alert and able to swallow.
Most important is to time the seizure and note the symptoms that occur. This will help the emergency professionals in assessing the situation and providing the correct treatment.
Note: Seizures usually end in a few minutes and most people will recover quickly and be able to continue with their normal activities. If the seizure lasts longer than 5 minutes, or if the person has difficulty breathing or has another medical emergency, call emergency services immediately.
Please Note: Every individual is different and prevention will also depend on underlying conditions and family history. Consultation with your doctor is recommended to understand what prevention strategies would be best for you.
If you need more guidance on the connection between stroke and seizures, please let us know.
References:
https://www.healthline.com/health/stroke
https://www.cdc.gov/epilepsy/communications/features/stroke.htm