Can chemotherapy cause heart failure?
Chemotherapy has revolutionized cancer treatment, offering hope and a fighting chance to countless individuals. However, like any powerful medical intervention, it comes with its own set of potential side effects and risks. One such risk that demands our attention is the association between chemotherapy and heart failure.
Studies have shown that heart failure due to chemotherapy affects about 5 to 15% of cancer patients. But the risks associated vary depending on the type of chemotherapy drugs used, their dosage and the underlying health conditions.

Chemotherapy-induced heart failure can occur when the drugs damage the heart muscle. Some drugs can cause inflammation or scarring of the heart muscle. Chemotherapy can also weaken the heart muscle by causing low blood count or anemia.
But heart failure due to chemotherapy can often be managed with medication and lifestyle changes. Talk to your doctor about the risks involved.
Your health is too important to ignore – schedule your appointment now.
Some measures to protect yourself from chemotherapy-induced heart failure are:
- Consult your doctor about the risks and benefits of different chemotherapy drugs.
- Ask about alternative methods to treat your cancer, such as targeted therapy or immunotherapy.
- Get regular checkups and heart tests during and after chemotherapy.
- Adopt a heart healthy diet and exercise regularly.
If you develop heart failure after chemotherapy, your doctor will develop a specific treatment plan. Treatment may include medication, lifestyle changes, or surgery.
How does chemotherapy lead to heart failure?
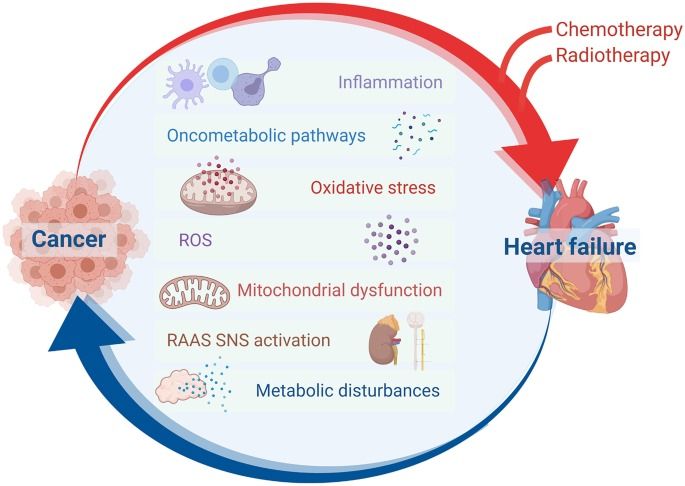
The specific mechanisms by which chemotherapy-induced heart failure occurs can vary depending on the drug used and your individual profile.
According to a study, individuals who received cancer treatment were found to have a threefold increased risk of developing heart failure within five years of their cancer diagnosis compared to those without cancer. Within 20 years, 10% of cancer survivors had developed heart failure compared to 6% of people without cancer.
Some of the ways in which your chemotherapy drugs can contribute to heart failure are:
- Cardiotoxicity: Some chemotherapy drugs are directly toxic to the heart muscle, leading to cardiotoxicity. This can weaken your heart's ability to pump blood effectively, eventually leading to heart failure. The occurrence of clinical heart failure seems to be in the range of 1% to 5%, and an asymptomatic decrease in heart function is in the range of 5% to 20%. Toxicity can occur as early as the first year.
- High doses: Chemotherapy in high doses can cause heart failure. Studies show that with the current maximum dosing limit, 7 in every 100 people who are given doxorubicin will develop heart failure.
- Oxidative Stress: Chemotherapy drugs can generate oxidative stress within the body, due to free radicals. This can damage heart cells and tissues, potentially leading to heart failure.
- Inflammation: Chemotherapy can trigger inflammatory responses. Chronic inflammation leads to changes in the structure and function of the heart muscle. This can over time cause heart failure.
- Reduced Blood Supply: Some chemotherapy drugs reduce the blood supply to the heart muscle. When the heart muscle is deprived of enough oxygen and nutrients, it can become weaker and less efficient at pumping blood.
- Electrolyte Imbalances: Imbalance between electrolytes potassium and calcium can cause irregular heart rhythms.
- Pre-existing cardiac issues: If you suffer from hypertension, atherosclerosis, or heart disease, you are more susceptible to chemotherapy-induced heart failure.
Discuss with your doctor the choice of chemotherapy drugs and the monitoring of cardiac function.
Take the first step to recovery. Get in touch with us for your treatment.
Let's take a look at some of the symptoms of heart failure that can be seen after chemotherapy.
What are the symptoms of heart failure during or after chemotherapy?
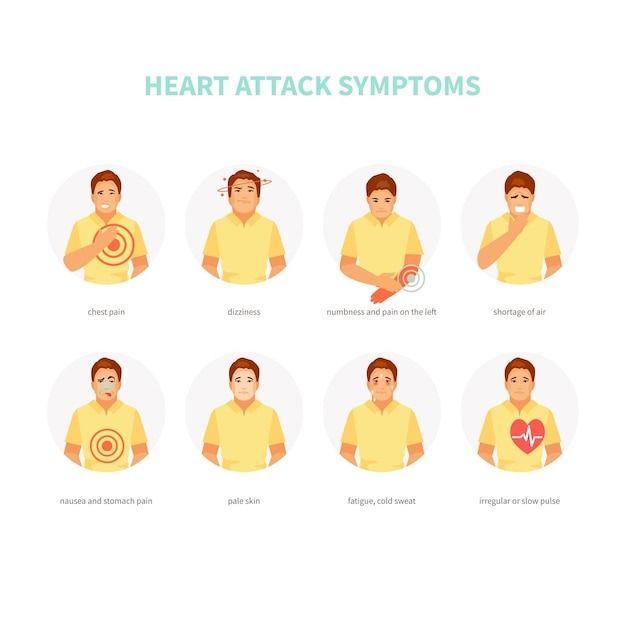
Some of the symptoms of heart failure during or after chemotherapy are:
- Shortness of Breath: Difficulty in breathing or shortness of breath, during physical activity or when lying down, is a common symptom of heart failure. This is because your heart's reduced ability to pump blood effectively.
- Fatigue: Unexplained and persistent fatigue or weakness which reduces your ability to perform daily activities.
- Swelling: Swelling in your legs, ankles, feet, or abdomen can occur due to fluid retention, commonly seen in heart failure.
- Rapid or Irregular Heartbeat: Heart palpitations, a racing heartbeat, or irregular heart rhythms may indicate heart issues.
- Persistent Cough: A chronic cough, with pink, frothy mucus, indicates fluid buildup in the lungs, a symptom of heart failure.
- Weight Gain: Sudden and unexplained weight gain, often due to fluid retention.
- Decreased physical activity: This may be seen without experiencing breathlessness or fatigue.
- Dizziness or Fainting: This can occur due to reduced blood flow to the brain, which may be related to heart dysfunction.
- Changes in Mental Alertness: Reduced blood flow to your brain can lead to confusion or difficulty in concentrating.
Wondering how this condition is treated? We have got you covered! Read more to find out.
How is chemotherapy-induced heart failure treated?
Look at the management strategies for chemotherapy-induced heart failure:
Treatment/Management | Description |
| Medicines | ACE inhibitors, Beta-blockers and Diuretics. |
| Cardiac Rehabilitation | To improve your heart health and quality of life. |
| Lifestyle Modifications | Dietary changes, like reduced salt intake, maintain a healthy weight, with regular, safe physical activity. Stop smoking |
| Fluid and Sodium Restriction | If you see severe fluid retention, then limit your fluid and sodium intake. |
| Regular Monitoring | Ongoing monitoring of cardiac function with echocardiograms. |
| Adjustments to Chemotherapy | Your doctor may modify the chemotherapy regimen. Decrease the dose of cardiotoxic drugs. Consider alternative treatments with lower cardiac risk. |
| Heart Transplant or Devices | If your case is severe and not responding to any medical therapy. |
Is it safe to continue chemotherapy if heart problems develop during treatment?
It depends on the following factors:
- Specific heart condition: Asymptomatic and mild cardiac problems may not require you to discontinue your chemotherapy.
- Severity of heart problems: If you show severe symptoms you will have to discontinue or modify the treatment (only as per your doctor's advice).
- Chemotherapy drugs being used: Some chemotherapy drugs are more harmful to the heart than others. If the heart problems are directly related to such a drug, then your doctors will change to a less cardiotoxic drug, which will still effectively treat your cancer.
- Continued monitoring: Regular echocardiograms and other cardiac tests can check your heart during chemotherapy.
- Cardioprotective Measures: Medicines or interventions may be used to minimize the impact of chemotherapy on the heart, allowing treatment to continue safely.
- Your overall health: If your cancer is at an advanced stage, then your doctor will find ways to manage the heart problems while continuing with a modified chemotherapy plan. Collaboration between your oncologists and cardiologists is required to develop your treatment plan.
Your well-being is our priority - call us to book your appointment today.
Is heart failure from chemotherapy reversible?
Generally, the reversibility of your chemotherapy-induced heart failure depends on various factors like:
- Early Detection: If heart problems are identified early, treatment measures can be implemented to prevent further damage and potentially reverse some of the effects.
- Severity of Cardiac Damage: Mild or moderate cardiac damage is more likely to be reversible with appropriate treatment, while severe damage may be more challenging to reverse completely.
- Specific Chemotherapy Drugs: Some chemotherapy drugs have a higher risk of causing reversible cardiac damage. Some drugs may even cause permanent damage to your heart. It can also depend on the dosage.
- Cardioprotective Measures: Cardioprotective medicine and procedures may improve your heart function. This could involve taking drugs like ACE inhibitors, beta-blockers, and lifestyle modifications.
- Overall Health: Your overall health, including other underlying diseases, can be a contributing factor.
- Recovery Period: Ongoing monitoring during the long recovery period is essential.
Sometimes, it can be reversed with timely intervention and appropriate treatment. But in case of failure of reversal, it may lead to permanent heart damage. Consult your medical practitioner for your personalized treatment.
References:






