According to the WHO, cancer is a leading cause of death worldwide. A 2020 survey revealed approximately 18.1 million new cases and 10 million deaths, which is about 1 in 6 deaths. The most common types of cancer are lung, breast, prostate, and colorectal cancer.
The statistics vary globally, but here are a few facts:
The most common types of cancer differ by region, for example -
- Lung and stomach cancer are more common in low-income countries.
- Breast and prostate cancer are more common in high-income countries.
- The number of new cancer cases is expected to rise to 27.5 million by 2040.
- Cancer is responsible for more deaths than tuberculosis, malaria, and HIV/AIDS combined.
- About 70% of all cancer deaths occur in low- and middle-income countries, where access to cancer care is often limited.
Please note that these statistics change constantly due to various factors, including cancer screening and early detection.
The advancements in cancer treatments like gene therapy offer the possibility of more effective and long-term treatments. Furthermore, these advanced techniques have fewer side effects compared to traditional chemotherapy and radiation therapy.
Would you like to know how gene therapy is revolutionizing cancer care? Read on to learn more about the role of gene therapy in cancer treatment.
Let's start by understanding the various types of gene therapy.
Types of gene therapy for cancer
| Therapy type | About Therapy |
Ex vivo gene therapy |
|
In vivo gene therapy |
|
In situ gene therapy |
|
Note: The selection of the appropriate method depends on the type of disease, the target cells, and the overall goal of the treatment. These methods are still in the research phase and under development.
Now that we know how gene therapy is delivered, let's find out what cancers this technique can be used for.
What type of cancer can be treated with gene therapy?
Gene therapy has the potential to treat a wide range of cancers by:
- introducing a functional copy of a gene
- by knocking down the expression of a gene that contributes to the development of the disease.
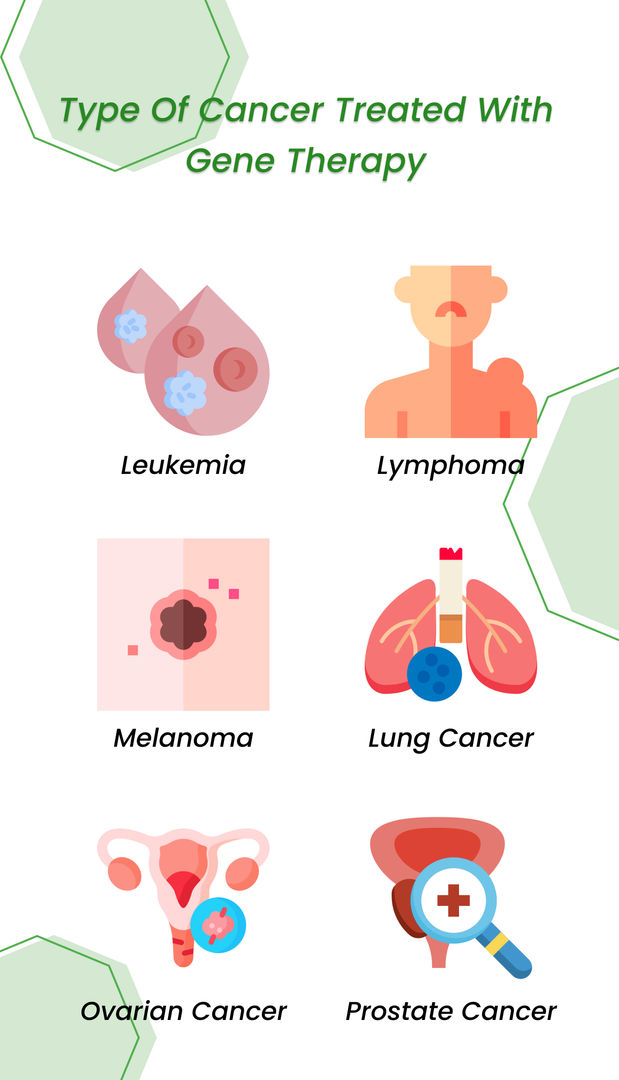
The most common types of cancer that are currently being researched and developed for gene therapy include:
- Certain types of leukemia, such as chronic lymphocytic leukemia (CLL) and acute lymphoblastic leukemia (ALL)
- Certain types of lymphoma, such as Hodgkin's lymphoma and non-Hodgkin's lymphoma
- Melanoma, which is a type of skin cancer
- Lung cancer
- Ovarian cancer
- Prostate cancer
Note: Many of these therapies are still in the early stages of research and development and have yet to be approved. Depending on the type, stage, and location of cancer, a combination of different therapies may be needed to achieve the best results.
Are you wondering too, as to how is gene therapy different from other cancer treatments like chemotherapy and radiation therapy?
Sean Marchese, MS, RN, is a registered nurse at The Mesothelioma Center with a background in oncology clinical trials has said that -
“Gene therapy differs from other cancer treatments, such as chemotherapy and radiation therapy, in that it specifically targets the genetic abnormalities that contribute to cancer growth rather than indiscriminately killing all rapidly dividing cells. These qualities make gene therapy potentially more precise and less toxic to healthy cells.”
Continue reading to understand how gene therapy is applied in cancer treatment.
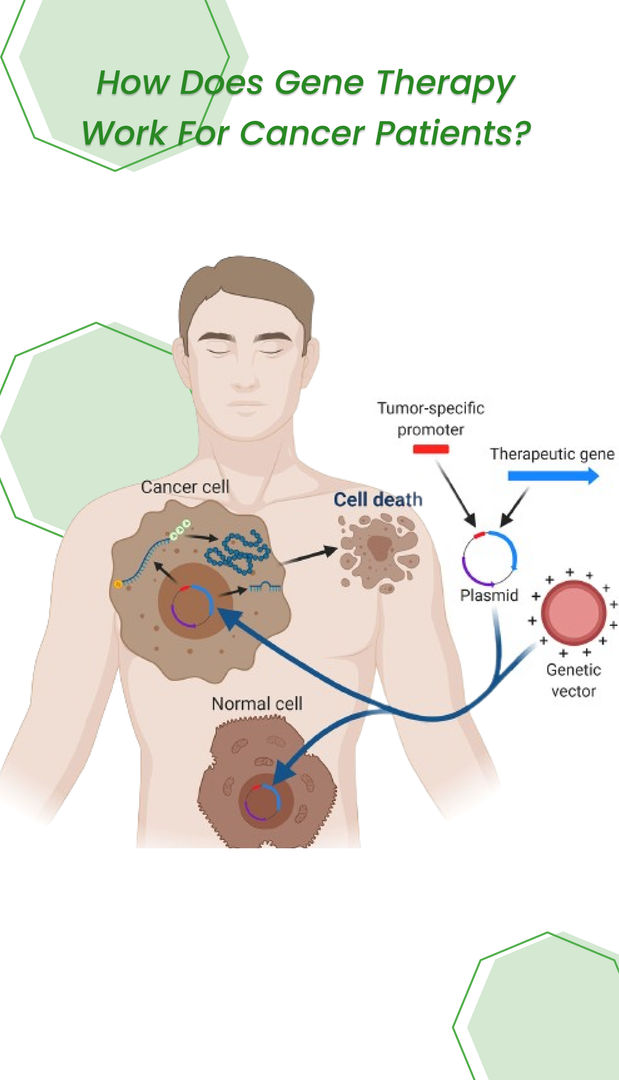
How is gene therapy given?
Gene therapy is typically delivered to the patient through the use of viral or non-viral vectors. A vector is a vehicle used to deliver genetic material to cells.
Viral vectors:
- Viral vectors are viruses that have been modified to carry corrective genetic material.
- They can be naturally occurring, like retroviruses and adenoviruses, or synthetic. The most common viral vectors used in gene therapy are adenoviruses, lentiviruses, and adeno-associated viruses
- The advantage of using viral vectors is that they can efficiently deliver genetic material to the cells. Still, they also have the potential to cause side effects and safety concerns.
Non-viral vectors:
- Non-viral vectors, as the name implies, are not derived from viruses. These vectors can be made from different materials, such as liposomes, plasmids, and nanoparticles.
- They offer a safer alternative to viral vectors, as they have a lower risk of causing side effects. However, they are less efficient at delivering genetic material to the cells.
The method of administration depends on the type of vector and disease. The vector can be delivered in the following ways:
- directly to the affected tissue through injection or intravenously
- through inhalation
- topical application
- oral administration
It's important to note that the delivery method is still a subject of research, and scientists are still working on developing new ways to increase the safety and efficiency of the treatment.
How successful is gene therapy for cancer?
The success rate of gene therapy in cancer varies depending on the type of cancer, the stage of the disease, and the specific therapy being used.
Some early clinical trials have shown promising results for certain types of cancer, such as leukemia, lymphoma, and melanoma, with patients experiencing significant improvements in their condition.
For example, some studies have shown that patients with acute lymphoblastic leukemia (ALL) who received gene therapy had a remission rate of up to 90%. Similarly, in some trials of CAR-T cell therapy for certain types of lymphoma and leukemia, remission rates of up to 80% have been reported.
Human cancer treatment with gene therapy offers an "opportunity of achieving for the long term." Improvements in gene transport to target cells and their "expression" are being prioritized in gene therapy for cancer. Ongoing clinical trials are being increasingly conducted.
That said, let’s take a look at a success story of a cancer patient who was given gene therapy treatment.
In an article published by The Guardian, a new gene therapy treatment successfully treated a 13-year-old patient with relapsed T-cell leukemia in the UK. The patient, Alyssa from Leicester, had previously undergone chemotherapy and a bone marrow transplant without success and had no remaining treatment options.

However, after receiving an infusion of donated T-cells modified using a technology called base editing, Alyssa is now in remission and recovering well. This pioneering treatment has raised hope that it could be used to help treat other childhood cancers and serious diseases in the future.
This certainly looks promising, doesn’t it? Medical experts and researchers are relentlessly paving their way to unlocking the potential of Gene Therapy.
Are there any risks involved in using gene therapy for cancer?
Genetic cancer treatment carries some possible risks. It's challenging to insert a gene right into your cells. So, it has to be typically sent via a carrier, also referred to as a vector.
Because viruses can identify specific cells and implant genetic data into the genes of these cells, they are the most prevalent vectors in gene therapy. Medical experts remove the viruses' primary damage-causing genes and replace them with the genes required to stop the disease.
The following risks are associated with this method:
Unintended immunological response: The recently introduced viruses may be attacked by your immune system since it perceives them as invaders. This may result in inflammation and, in extreme circumstances, organ failure.
Targeting healthy cells: The modified viruses will likely infect other cells in addition to the targeted cells that carry mutant genes. If this occurs, healthy cells might be harmed, leading to additional illnesses or a new tumor.
Viral infection: It's likely that once the viruses are inside the body, they will regain their capacity to wreak disease.
Please note that the risk of these potential side effects varies depending on the specific type of Gene therapy being used and the stage of the cancer being treated.

So what are you waiting for?
References:
Taking Stock of CAR T-Cell Therapy | Cancer Today (cancertodaymag.org)






