Overview
Prostate cancer is one of the most common cancers among men worldwide. While a prostatectomy—surgical removal of the prostate gland—is an effective treatment for many, there is still a chance that cancer may return. This is known as recurrent prostate cancer.
After prostatectomy, about 20-40% of patients experience a rise in PSA levels (biochemical recurrence) within 10 years, usually around 20-38 months after surgery. A PSA level of 0.2 ng/mL or higher, followed by another increase, is considered a sign of recurrence.
Early detection makes all the difference! Book an appointment with an urologist for expert advice.
What Is Recurrent Prostate Cancer?
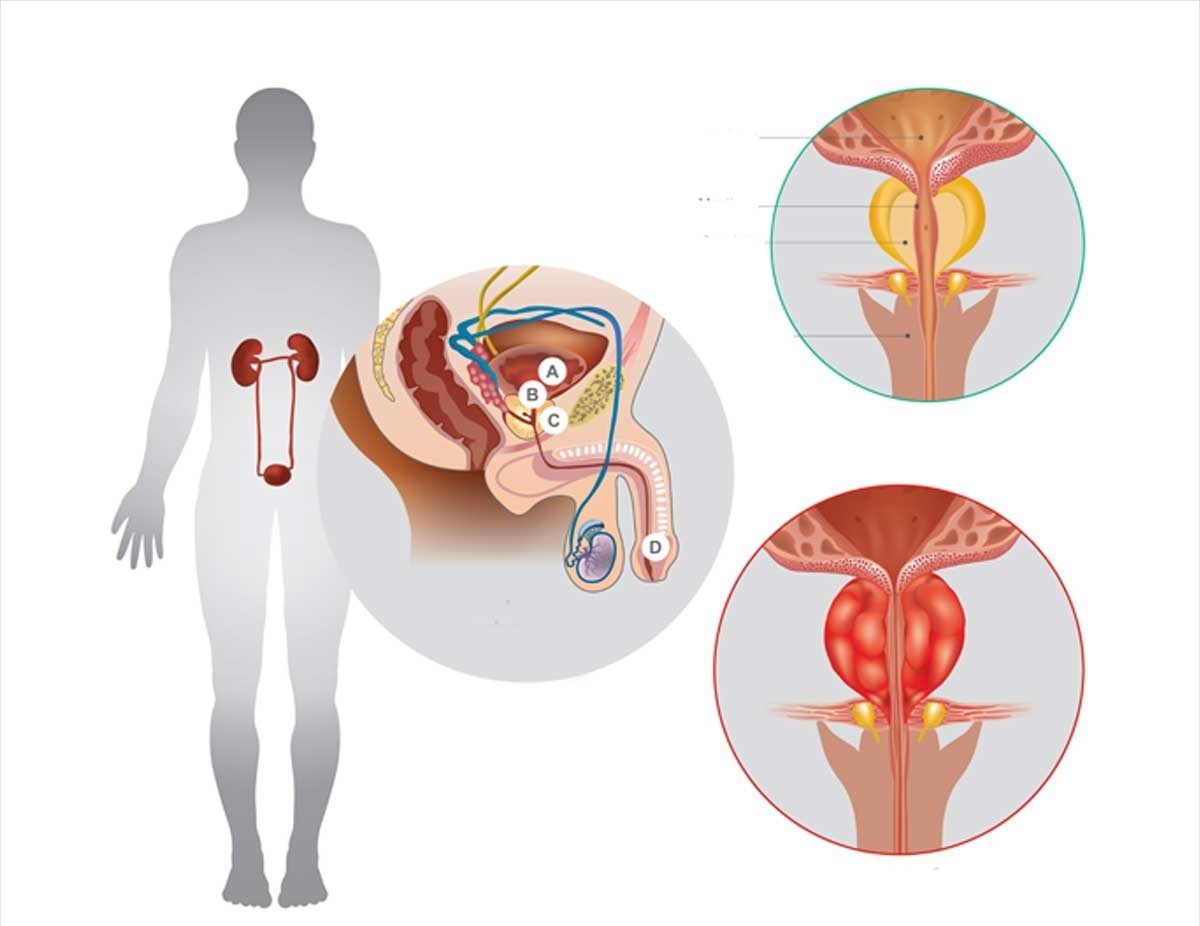
Recurrent prostate cancer refers to cancer that reappears after the prostate has been surgically removed (radical prostatectomy).
Even though prostate surgery can be successful, some cancer cells may remain and grow over time, leading to a recurrence. This can happen either near the prostate (local recurrence) or in other areas like the bones or organs (distant recurrence).
Staying informed and following up with your doctor regularly helps catch and manage these situations early!
Early Signs of Recurrent Prostate Cancer
Some of the early signs of recurrent prostate cancer after prostatectomy are as follows:
- Rising PSA Levels: Monitoring prostate-specific antigen (PSA) levels is crucial. A steady or rising trend in PSA levels may indicate recurrent prostate cancer. PSA is a protein made by prostate cells. Normally, PSA should be very low after surgery. If PSA levels start going up, it could mean the cancer is back, a situation often referred to as recurrent prostate cancer after prostatectomy.
Urinary Changes: Changes in urinary habits, such as increased frequency, urgency, or difficulty in initiating or stopping the flow, can be indicative of recurrent prostate cancer.
Blood in Urine or Semen: Hematuria (blood in urine) or hemospermia (blood in semen) may be early signs of recurrence. If you notice any unusual blood, talk to your doctor for prompt evaluation.
Erectile Dysfunction: Recurrent prostate cancer may impact erectile function. If you're having trouble getting or keeping an erection, it's a sign that needs attention. Talk to a doctor about it.
Bone Pain: Metastasis to the bones is common in recurrent prostate cancer. Persistent or unusual bone pain, specially in the back, hips, or pelvis indicates a chance of recurrence.
Rapid Weight Loss: Significant unintentional weight loss can be associated with various cancers, including recurrent prostate cancer. It's important to investigate the cause.
Early detection, regular follow-ups, and consultations with your doctor are important for effectively managing and improving outcomes in recurrent prostate cancer.
Discover the curative and control treatments that can make a difference!
Several factors can contribute to the recurrence of prostate cancer after prostatectomy:
- Positive Surgical Margins: If cancer cells are found at the edges of the removed tissue, it indicates that not all of the cancerous tissue was removed during surgery.
- High-Grade Tumors: Aggressive or high-grade tumors are more likely to recur, as they have a higher potential for spreading or growing back after treatment.
- Elevated PSA Levels: Prostate-specific antigen (PSA) is a protein produced by prostate cells. After prostatectomy, PSA levels should drop to undetectable levels. If PSA begins to rise, it can be a sign of recurrence.
- Cancer Stage at Diagnosis: Patients with advanced or more aggressive cancer at the time of diagnosis have a higher chance of recurrence.
- Micrometastasis: Small groups of cancer cells that were not detected during initial treatment may have already spread to other parts of the body, causing recurrence.
Want to know what can cause prostate cancer to come back? Let’s find out.
Risk Factors for Recurrence
- High Preoperative PSA Levels: Higher PSA before surgery increases the risk of recurrence.
- Positive Surgical Margins: If cancer cells are found at the edge of the removed tissue, the risk of recurrence is higher.
- Advanced Tumor Stage: The more advanced the cancer at the time of surgery, the higher the chance of recurrence.
- High Gleason Score: A Gleason score of 8-10 indicates more aggressive cancer, increasing recurrence risk.
- Lymph Node Involvement: If the cancer has spread to the lymph nodes, recurrence is more likely.
- Seminal Vesicle Invasion: If cancer is found in the seminal vesicles, the risk of recurrence is higher.
- Short PSA Doubling Time: A rapidly rising PSA level after surgery indicates a higher risk of recurrence
Wondering how the recurrence of prostate cancer is detected? Find out here!
How Is Recurrent Prostate Cancer Detected?
Recurrent prostate cancer is often first suspected when PSA levels begin to rise after surgery. PSA tests are typically done regularly after prostatectomy to monitor for any signs of recurrence. If elevated PSA levels are detected, additional tests may be recommended, such as:
- Imaging scans: CT scans, MRIs, bone scans, or PET scans may be used to identify where the cancer has returned.
- Biopsy: In some cases, a biopsy may be performed to confirm the presence of recurrent cancer.
Treatment Options for Recurrent Prostate Cancer After Prostatectomy
Treatment for recurrent prostate cancer depends on several factors, including where the cancer has returned, how aggressive it is, and the patient’s overall health. Common treatment options include:
1. Radiation Therapy
Radiation therapy is often the first line of treatment for patients whose cancer has recurred in the prostate bed (the area where the prostate was located). Radiation can target any remaining cancer cells that were not removed during surgery.
2. Hormone Therapy
Hormone therapy, also known as androgen deprivation therapy (ADT), reduces the levels of male hormones (androgens) that prostate cancer cells rely on to grow. This treatment is often used when cancer has spread beyond the prostate bed or if radiation therapy is not effective.
3. Chemotherapy
Chemotherapy may be recommended for advanced recurrent prostate cancer, particularly when the cancer has spread to other parts of the body and hormone therapy is no longer effective.
4. Immunotherapy
Immunotherapy is a newer approach to treating recurrent prostate cancer. It works by boosting the body’s immune system to recognize and attack cancer cells. Sipuleucel-T (Provenge) is one example of an immunotherapy approved for advanced prostate cancer.
5. Targeted Therapy
Targeted therapy focuses on specific genetic mutations in cancer cells. In cases of recurrent prostate cancer, drugs like PARP inhibitors may be used for patients with certain genetic mutations, such as BRCA1 or BRCA2 mutations.
6. Active Surveillance
In some cases, particularly when the recurrence is slow-growing and not causing symptoms, doctors may recommend active surveillance. This approach involves closely monitoring the patient’s PSA levels and symptoms without immediate treatment.
Let’s learn how to prevent and manage prostate cancer recurrence.
Prevention and Management of Recurrence
The prognosis for recurrent prostate cancer varies depending on how early the recurrence is detected, the treatment used, and the aggressiveness of the cancer. Many men with recurrent prostate cancer can still live for many years, especially if the recurrence is detected early and treated effectively.
It’s essential for patients who have undergone a prostatectomy to continue regular follow-ups with their doctor and monitor PSA levels as directed. Early detection and prompt treatment of recurrence can significantly improve outcomes.
FAQs
1. Can recurrent prostate cancer be cured?
While a complete cure for recurrent prostate cancer is challenging, it can often be effectively managed, especially if caught early. Treatment options like radiation therapy, hormone therapy, and others can control the disease and prolong survival.
2. How often should PSA be checked after prostatectomy?
After prostatectomy, PSA levels are typically monitored every 3-6 months for the first few years, and less frequently thereafter, depending on the patient’s risk factors and PSA levels.
3. What are the chances of recurrence after prostatectomy?
The likelihood of recurrence depends on various factors, such as the cancer stage at diagnosis, the surgical margins, and whether PSA levels remain undetectable after surgery. On average, 20-40% of patients experience recurrence within 10 years.






